Pandemic at a perspective
- Himanshu Sadulwad
- Feb 6, 2024
- 5 min read
Author: Himanshu Sadulwad
'On 31 December 2019, the WHO China Country Office was informed of a pneumonia of unknown cause, detected in the city of Wuhan in Hubei province, China.'
No human would have imagined that these cases would lead to a full blown global pandemic. As the pandemic now enters its third year let's take a look back at the steps which led to this disaster.
Origin
Following the initial report of these pneumonia cases in China, on 4th January 2020 WHO responded to the cluster of pneumonia cases to track the situation and provide information as it emerged. Following this, guidelines were released with reference to SARS and MERS and on 11th January 2020 the first case of this novel coronavirus outside China was confirmed in Thailand. Field visits were made to Wuhan to discuss the screening procedures at airports to limit the spread of the virus. The genome of the novel coronavirus was made publicly available on 11th January 2020. On 30th January 2020 WHO Director-General Dr. Tedros Ghebreyesus declared the novel coronavirus outbreak a Public Health Emergency of International Concern. On 11th February 2020 WHO announced that the disease caused by the novel coronavirus would be named COVID-19. The decision to not let the disease be named after a person or region was to prevent any stereotypes which may arise due to the name.The events that followed included release of guidelines by the WHO, multiple preventive measures and general information about the disease was released to educate the masses. This period also saw the spread of the disease outside China and a spike in the number of cases.
"Pandemic is not a word to use lightly or carelessly. It is a word that, if misused, can cause unreasonable fear, or unjustified acceptance that the fight is over, leading to unnecessary suffering and death."
On 11th March 2020 concerned by the alarming levels of spread and severity, and by the alarming levels of inaction, WHO officially declared that COVID-19 could be characterized as a pandemic.
Following this massive announcement, countries stepped up their resolutions to combat the virus. Curfews and lockdowns were implemented to reduce its spread. Our major weapon to limit the spread of this disease was and remains to this day 'mask'. Let us evaluate how the use of a mask helped reduce cases and the stigma surrounding it.
Masks
Need for masks
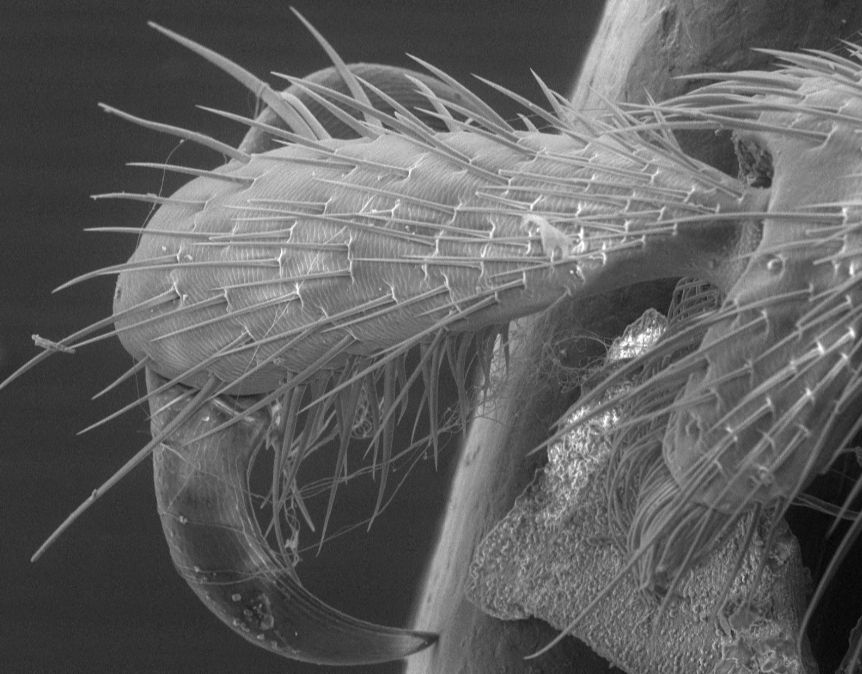
Among all plausible routes, airborne transmission of SARS-CoV-2 via respiratory droplets and aerosols is responsible for the rapid spread of COVID-19. Respiratory droplets, which have a relatively large size of 5–10 μm, are emitted when an infected individual coughs or sneezes. In comparison, aerosols are nuclei of respiratory droplets that form after evaporation, and are usually less than 5 μm in size. Viral particles have been found in respiratory droplets and exhaled aerosols of infected individuals, and are bound to inhalable aerosols in the atmosphere. Accumulating evidence suggests that respiratory droplets and aerosols expelled during a sneeze or cough can travel up to 12 to 26 feet, significantly farther than the 6-ft social distancing guideline recommended by the Centers for Disease Control and Prevention (CDC) of the United States. Due to their small size and hence negligible influence by gravity, aerosols generally remain afloat in the air for prolonged periods of time, causing an additional threat of airborne transmission, especially in indoor environments with poor ventilation.

This is where the use of masks comes into the picture. This simple and low-cost method is highly effective at mitigating virus transmission. Reducing disease spread requires two things: limiting contacts of infected individuals via physical distancing and other measures and reducing the transmission probability per contact. The preponderance of evidence indicates that mask wearing reduces transmissibility per contact by reducing transmission of infected respiratory particles in both laboratory and clinical contexts. Public mask wearing is most effective at reducing spread of the virus when compliance is high. By the end of June 2020, nearly 90% of the global population lived in regions that had nearly universal mask use, or had laws requiring mask use in some public locations, and community mask use was recommended by nearly all major public health bodies. This was a radical change from the early days of the pandemic, when masks were infrequently recommended or used.
Efficacy of the usage of masks
If there is strong direct evidence, either a suitably powered randomized controlled trial (RCT),a suitably powered metaanalysis of RCTs, or a systematic review of unbiased observational studies that finds compelling evidence, then that would be sufficient for evaluating the efficacy of public mask wearing, at least in the contexts studied.
Cochrane and the World Health Organization both point out that, for population health measures, we should not generally expect to be able to find controlled trials, due to logistical and ethical reasons, and should therefore instead seek a wider evidence base. This issue has been identified for studying community use of masks for COVID-19 in particular. Therefore, we should not be surprised to find that there is no RCT for the impact of masks on community transmission of any respiratory infection in a pandemic.
The Australian influenza RCT and the Beijing households observational trial found around 80% efficacy among compliant subjects, and the one SARS household study of sufficient power found 70% efficacy for protecting the wearer. A Cochrane review on physical interventions to interrupt or reduce the spread of respiratory viruses included 67 RCTs and observational studies. It found that “overall masks were the best performing intervention across populations, settings and threats.”
Multiple studies offer evidence in favor of widespread mask use as source control to reduce community transmission. Nonmedical masks use materials that obstruct particles of the necessary size; people are most infectious in the initial period postinfection, where it is common to have few or no symptoms; nonmedical masks have been effective in reducing transmission of respiratory viruses; and places and time periods where mask usage is required or widespread have shown substantially lower community transmission. Models suggest that public mask wearing is most effective at reducing spread of the virus when compliance is high.
The Swiss Cheese Model
The Swiss cheese model of accident causation is used in risk analysis and risk management. This model was originally proposed by James Reason.
The metaphor itself is easy enough to grasp; multiple layers of protection, imagined as cheese slices, block the spread of SARS CoV-2. No one layer is perfect; each has holes, and when the holes align, the risk of infection increases. But several layers combined — social distancing, masks, hand-washing, testing and tracing, ventilation, government messaging, vaccination — significantly reduce the overall risk.

Note that in the figure the 'misinformation mouse' is nibbling holes which weakens the barriers, leaving us vulnerable.
The main feature of a Swiss cheese model is that a single layer doesn't guarantee protection as it has its shortcomings and errors, 'holes'. In order to intensify our protection we need multiple such layers. This way we can minimize our risk of contracting the virus.
References
Reason, J. “Human error: models and management.” BMJ (Clinical research ed.) vol. 320,7237 (2000): 768-70. doi:10.1136/bmj.320.7237.768
Ju, Jerry T J et al. “Face masks against COVID-19: Standards, efficacy, testing and decontamination methods.” Advances in colloid and interface science vol. 292 (2021): 102435. doi:10.1016/j.cis.2021.102435
Howard, Jeremy et al. “An evidence review of face masks against COVID-19.” Proceedings of the National Academy of Sciences of the United States of America vol. 118,4 (2021): e2014564118. doi:10.1073/pnas.2014564118
Cowling B. J., et al. , Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 5, E279-E288 (2020)
Higgins J. P., et al. , Cochrane Handbook for Systematic Reviews of Interventions (John Wiley, 2019)
Wang Y., et al. , Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: A cohort study in Beijing, China. BMJ Global Health 5, e002794 (2020)


Comments