An Insight into Cervical Cancer
- Himanshu Sadulwad
- Feb 5, 2024
- 9 min read
Author: Katie Bean
Introduction
January marks cervical cancer awareness month, and it has never been more important to shed light on seventh most common type of cancer (Manikandan et al. 2019, 314). Mainly affecting women or anyone with a cervix under the age of 45, cervical cancer is usually caused by HPV (human papilloma virus) infections. Though this form of cancer can indeed be fatal, it is extremely treatable if caught in early stages through screening, and largely preventable owing to the development of HPV vaccines. Raising awareness for cervical cancer encourages screening and vaccination and also helps to promote research and implement these essential screening and vaccination programmes in lower income countries.
Aetiology and Pathogenesis
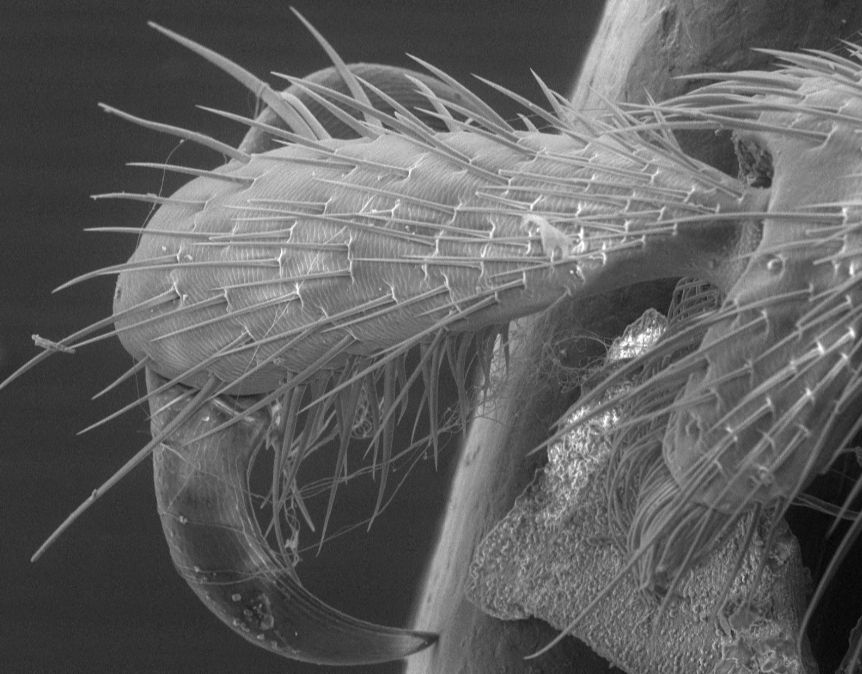
Most cases of cervical cancer result from infection with the HPV virus. There are two particular strains of HPV that are associated with cervical carcinoma: HPV-16 and HPV-18. The earliest transformation of healthy cells into cancerous occurs in a region called the squamocolumnar junction (see figure 1). The premalignant transformation of cells in this region is termed cervical intraepithelial neoplasia (CIN) - the severity of which is systematically graded (see figure 2). For carcinogenesis to occur, HPV viral proteins must alter the host cells. The oncoproteins most responsible for this are called E6 and E7 - they prevent the function of the p53 tumour suppressor gene, allowing uncontrolled cell proliferation. Once the cells have become cancerous, angiogenesis (blood vessel formation) can occur, allowing tumours to grow and metastasize - thus exacerbating the condition.
Risk factors
There are a number of risk factors that might increase the chance that an individual develops cervical cancer. Essentially all people that are sexually active will ultimately become infected with HPV in their lives. These short-term, less aggressive infections are not the cause of cervical cancer, rather it is the higher risk, previously mentioned strains that hold responsibility. Therefore, one of the most significant risk factors for developing cervical cancer is having multiple sexual partners, as it increases the chance that an individual may become infected with a high-risk strain. Individuals that are also at a higher risk are the immunocompromised; if someone has a weakened immune system, it is harder for them to fight off a more persistent HPV infection. Smoking is also a pertinent risk factor; it has been hypothesised that the by-products of tobacco can damage DNA within cervical cells and that smoking reduces the capability of the immune system to respond to HPV. (National Cancer Institute 2023) However, the precise molecular mechanisms by which this occurs are yet to be proven - more research is needed to do so. (Castle 2008, 6084) Long-term use of oral contraceptives is also associated with increased risk - the risk increases by a factor of 1.9 for every 5 years of oral contraceptive use. (Johnson et al. 2019, 166-174) Again, the molecular mechanisms behind this association is not well understood. (National Cancer Institute 2023)
Preventative Measures
In 2018, the WHO initiated a global call for action focussing on the elimination of cervical cancer. This was followed by the Global Strategy to Accelerate the Elimination of Cervical Cancer put forward by the World Health Assembly. The Strategy proposes three central goals to achieve this - vaccination, screening and treatment. More specifically, the Strategy aims to have 90% of girls fully vaccinated with the HPV vaccine by the age of 15 and 70% of women screened using a high-performance test by the age of 35, and again by the age of 45 (The Lancet Regional Health – Americas 2017). In the UK, the vaccine offered by the NHS is called Gardasil 9, and is recommended around 12-13 (before an individual becomes sexually active) (GOV.UK 2023). The vaccine works by action of virus-like particles (VLPs), which induce antibody production. Upon reinfection with the actual virus, these antibodies prevent the HPV from entering and infecting the basal cells of the epithelium. (Harper, Vierthaler, and Santee 2010, 2) One of the reasons that the HPV vaccine has been found to be highly effective is due to the strong immunogenic nature of the virus-like particles; they stimulate high levels of antibody production (National Cancer Institute 2021). Condoms (an example of a physical barrier method) are also able to reduce the risk of HPV transmission between individuals, though infection can still occur in areas of skin that are exposed during intercourse. (National Cancer Institute 2023)
Screening for Cervical Cancer
Since cervical cancer is such a preventable disease, it is imperative to emphasise the importance of available screening procedures; these ensure the detection of abnormal cells, thus preventing the development of cervical cancer. The traditional method of cervical screening is a Pap smear (named after the Greek physician Georgios Papanikolaou). The procedure, that lasts no longer than 5 minutes, involves the insertion of a speculum and soft brush into the cervix to take a sample of cells. This service is available to women and those with a cervix aged 25-64 in England (NHS 2024). The Pap smear allows for detection of HPV - if present, this can be followed by a cytology test to check for abnormal cells. If abnormal cells are detected, the patient is referred for a colposcopy (GOV.UK 2024). During a colposcopy, a colposcope (lighted microscope) enables the magnification of cervical tissue. (Cleveland Clinic 2022). If a precancerous lesion is identified, a ‘large loop excision of the transformation zone’ is performed - this removes the precancerous cells, inhibiting development. (Burmeister et al. 2022)
Disease management
Treatment for cervical cancer varies depending on the progression of the tumour, as well as the health and preference of the patient (for example, if they desire to preserve fertility). In early stages of the disease, surgical procedures are able to remove the carcinoma. Microinvasive disease can be treated with conisation (the removal of a ‘cone-shaped portion’ of the cervix) (Cooper et al. 2023), as well as a simple trachelectomy (removal of the cervix). (Circle Health Group 2024). The aforementioned procedures are fertility-sparing, though a simple hysterectomy can also be performed if the patient does not desire to preserve fertility (Marth et al. 2017, 76-77). larger tumours require radical hysterectomy with bilateral lymph node dissection (the latter is used to assess whether cancer cells have spread to the lymph nodes of the pelvis - this would increase the risk of metastasis) (Marth et al. 2017, 76). Radiotherapy and chemotherapy are employed in more advanced stages of the disease (e.g., when the cancer has metastasised) (Marth et al. 2017, 77). Radiotherapy and chemotherapy can also be used as adjuvant therapy (this is administered after treatment to reduce the chance of the cancer returning) (Mayo Clinic 2024). Chemotherapy is often used palliatively, with the aim of improving the quality of life for terminal patients (Johnson et al. 2019, 170).
Raising Awareness
Although HPV infection, and ultimately cervical cancer, is largely preventable, there are various socioeconomic factors that reduce the efficiency of screening. A study on cervical cancer in Central and South America concluded that poverty is the most significant factor in the incidence of and deaths from the disease globally. (Murillo et al. 2016, 5). Economic determinants are significant particularly regarding access to medical resources for screening. For example, developed countries tend to have a higher standard of experimental conditions, enabling higher sensitivity for Pap smear analysis (usually 80-90%). In areas that have less sophisticated conditions, the sensitivity is limited to around 30-40% (Zhang et al. 2020, 724). There are other barriers that reduce access to screening, such as cultural beliefs and anxiety around gynaecological examinations; these factors tend to be more prevalent in low and middle-income countries (The Lancet Regional Health – Americas 2017). A general lack of awareness is also a crucial barrier; a 2018 study conducted in India investigated 100 female students between the ages of 18 and 24 found that only 5 individuals were aware about causes and risk factors regarding cervical cancer. 96 individuals were unaware about Pap testing or the HPV vaccine (Manikandan et al. 2019, 318).
However, in order to align with the WHO’s global call, programmes are being implemented to overcome this. For example, the HOPE project in Peru recruits women from disadvantaged communities to spread information about HPV to women aged 30 and 49 years old (HOPE PERU 2024). They additionally provide self-sampling tests to women and follow the tests up with analysis, collaborating with a network of expert gynaecologists (HOPE PERU 2024). The HOPE ladies were successfully able to increase awareness in their community, the participation rate increased to 94% owing to their efforts. The success of this programme could potentially lead to similar schemes being implemented in other countries (The Lancet Regional Health – Americas 2017).
Developments in Screening and Treatment
As previously mentioned, there are a number of socioeconomic factors that act as barriers to cervical cancer screening. One particular manifestation of this is reduced sensitivity of Pap smear analysis, though an alternative method, liquid-based cytology is able to overcome this limitation. Its higher sensitivity enables cervical abnormalities to be detected despite less sophisticated experimental conditions (Zhang et al. 2020, 724). Regarding treatment, immunotherapy is fast becoming a useful method for managing cervical cancer. It focuses on targeting ‘checkpoints’ which can be turned on or off to stimulate an immune response; cancer cells often manipulate these to evade immune recognition. Drugs that inhibit these checkpoints are therefore able to treat cervical cancer (Johnson et al. 2019, 170). Pembrolizumab is an example of a drug that targets a checkpoint, the checkpoint in question being that between the two proteins PD-1 and PD-L1. Some tumours express protein PD-L1 at a high level, and when PD-L1 upon interaction with PD-1, it prevents T-cells from destroying the cancerous cells. Pembrolizumab works by inhibiting this interaction, enabling T-cells to efficiently destroy the tumour cells (Flynn and Gerriets 2023). In an article written in March 2023, the Royal Marsden announced pembrolizumab as the first approved immunotherapy treatment for cervical cancer provided by the NHS (under the name of Keytruda). It is administered in combination with chemotherapy to patients suffering with advanced-stage cervical cancer, where the cancer has not responded to previous treatments (The Royal Marsden 2023).
Conclusion
Overall, cervical cancer month functions as an essential reminder of the importance of raising awareness for one of the most common cancers globally. Measures such as screening and vaccination allow the detection and monitoring of HPV infections, though barriers to this prove to be hugely prevalent in countries with lower income. By implementing programmes such as the HOPE project in Peru and investing in research into more comprehensive analysis techniques and treatment, the risk of cervical cancer can be significantly reduced. There is still a long way to go in the journey towards cervical cancer elimination, but building on these advances could ensure a future free of cervical cancer.
References
Burmeister, Carly A., Saif F. Khan, Georgia Schaefer, Nomonde Mbatani, Tracey Adams, Jennifer Moodley, and Sharon Prince. 2022. “Cervical cancer therapies: Current challenges and future perspectives.” Tumour Virus Research 13, no. 13 (June): 13. 10.1016/j.tvr.2022.200238.
Castle, Philip E. 2008. “How Does Tobacco Smoke Contribute to Cervical Carcinogenesis?” Journal of Virology 82, no. 12 (June): 6084–6086. 10.1128/JVI.00103-08.
Circle Health Group. 2024. “Fertility Sparing Treatment (Trachelectomy) for Cervical Cancer.” Circle Health Group. https://www.circlehealthgroup.co.uk/treatments/cervical-cancer-fertility-sparing-treatment.
Cleveland Clinic. 2022. “Colposcopy: Biopsy, Purpose, Procedure, Risk & Results.” Cleveland Clinic. https://my.clevelandclinic.org/health/diagnostics/4044-colposcopy.
Cooper, Danielle B., Jose Carungno, Charles J. Dunton, and Gary W. Menefee. 2023. “Cold Knife Conization of the Cervix - StatPearls.” NCBI. https://www.ncbi.nlm.nih.gov/books/NBK441845/.
Flynn, James P., and Valerie Gerriets. 2023. “Pembrolizumab - StatPearls.” NCBI. https://www.ncbi.nlm.nih.gov/books/NBK546616/.
GOV.UK. 2023. “Information on the HPV vaccination from September 2023.” GOV.UK. https://www.gov.uk/government/publications/hpv-vaccine-vaccination-guide-leaflet/information-on-the-hpv-vaccination-from-september-2023.
GOV.UK. 2024. “Cervical screening: programme overview.” GOV.UK. https://www.gov.uk/guidance/cervical-screening-programme-overview.
Harper, Diane M., Stephen L. Vierthaler, and Jennifer A. Santee. 2010. “Review of Gardasil.” J Vaccines Vaccin 1, no. 107 (November): 107. 10.4172/2157-7560.1000107.
HOPE PERU. 2024. “THE PROJECT – HOPE PERU.” HOPE PERU. https://hopeperuproject.org/project/.
Johnson, Cynae A., Deepthi James, Amelita Marzan, and Mona Armaos. 2019. “Cervical Cancer: An Overview of Pathophysiology and Management.” Seminars in Oncology Nursing 35, no. 2 (April): 166-174. https://doi.org/10.1016/j.soncn.2019.02.003.
The Lancet Regional Health – Americas. 2017. YouTube: Home. https://www.sciencedirect.com/science/article/pii/S2667193X22000783.
Manikandan, Saranya, Subasish Behera, Nageswarao M. Naidu, Vignesswary Angamuthu, Omar Mohammed, and Abhitosh Debata. 2019. “Knowledge and Awareness Toward Cervical Cancer Screening and Prevention Among the Professional College Female Students.” J Pharm Bioallied Sci 2019 May, no. 11 (May): 314-320. 10.4103/JPBS.JPBS_21_19.
Marth, C., F. Landoni, S. Manher, A. Gonzalez-Martin, and N. Columbo. 2017. “Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up.” Annals of Oncology 28, no. 4 (July): 72-83. https://doi.org/10.1093/annonc/mdx220.
Mayo Clinic. 2024. “Adjuvant therapy: Treatment to keep cancer from returning.” Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/cancer/in-depth/adjuvant-therapy/art-20046687.
Murillo, R., R. Herrero, M. S. Sierra, and D. Forman. 2016. “Etiology of cervical cancer (C53) in Central and South America.” International Agency for Research on Cancer.
National Cancer Institute. 2021. “Human Papillomavirus (HPV) Vaccines - NCI.” National Cancer Institute. https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-vaccine-fact-sheet.
National Cancer Institute. 2023. “Cervical Cancer Causes, Risk Factors, and Prevention.” National Cancer Institute. https://www.cancer.gov/types/cervical/causes-risk-prevention.
NHS. 2024. “Cervical screening.” NHS. https://www.nhs.uk/conditions/cervical-screening/.
The Royal Marsden. 2023. “Immunotherapy available to NHS cervical cancer patients for the first time.” The Royal Marsden. https://www.royalmarsden.nhs.uk/news-and-events/news/immunotherapy-available-nhs-cervical-cancer-patients-first-time.
Zhang, Shaokai, Huifang Xu, Luyao Zhang, and Youlin Qiao. 2020. “Cervical cancer: Epidemiology, risk factors and screening.” Chinese Journal of Cancer Research 32, no. 6 (December): 720-728. 10.21147/j.issn.1000-9604.2020.06.05.


Comments